Introduction
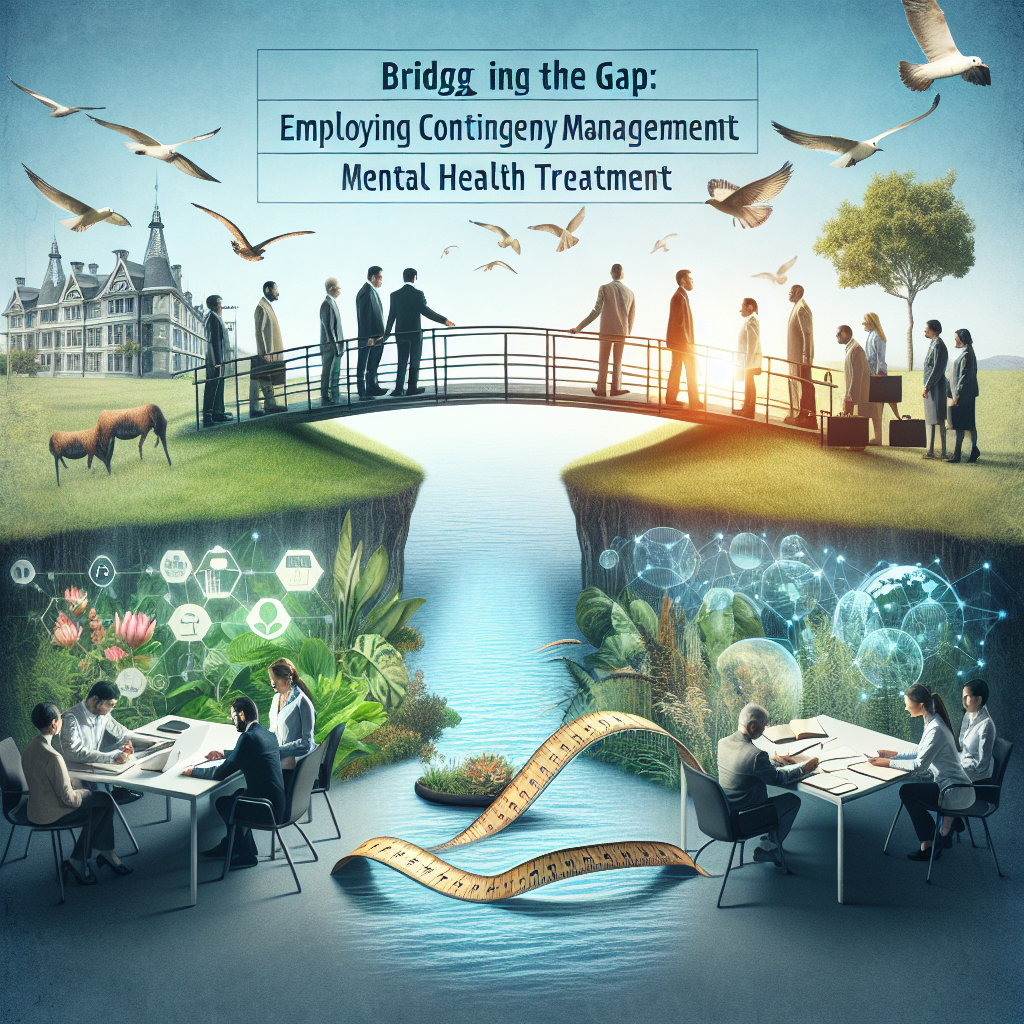
In an era where mental health challenges are increasingly recognized yet often unmet, innovative treatment approaches are more essential than ever. One such approach is contingency management, a technique that offers tangible rewards for positive behaviors, effectively “bridging the gap” in mental health treatment. This article delves into the vital role contingency management plays in overcoming barriers to effective mental health care, supported by case studies, data, and practical insights.
The Foundation of Contingency Management
What is Contingency Management?
Contingency management (CM) is a behavioral therapy strategy strongly rooted in the principles of operant conditioning. By reinforcing desired behaviors with tangible incentives, this approach is particularly effective in promoting adherence to treatment protocols and encouraging positive lifestyle changes. In this section, we will explore the foundational elements of CM, setting the stage for its application in mental health treatments.
Key Principles of Contingency Management
Reinforcement of Positive Behavior: CM focuses on encouraging desirable behaviors while providing immediate rewards, which enhances motivation.
Structured Framework: CM operates within a clearly defined structure, ensuring that clients understand the behaviors that will be rewarded.
- Flexibility and Customization: Unlike one-size-fits-all programs, CM allows for the customization of rewards and goals, making it suitable for diverse populations.
Evidence Supporting Contingency Management
Multiple studies illustrate the efficacy of contingency management in treating addiction, depression, anxiety, and other mental health issues. For instance, research published in JAMA Psychiatry demonstrates that individuals undergoing CM for substance use disorders showed significantly higher abstinence rates compared to those receiving standard treatments.
Bridging the Gap in Mental Health Care
Identifying Barriers to Effective Treatment
Despite advancements in mental health awareness, numerous barriers continue to impede effective treatment:
Stigma: Negative perceptions of mental health disorders discourage individuals from seeking help.
Access to Services: Many communities lack the necessary resources or trained professionals.
- Treatment Adherence: Psychological conditions often challenge individuals’ motivation, making adherence to treatment complex.
By strategically employing contingency management, practitioners can directly address these barriers, fostering an environment conducive to lasting change.
How Contingency Management Addresses These Barriers
Case Study: Contingency Management in Substance Use Treatment
A notable application of CM can be observed in a recent program aimed at treating substance use disorders. In a clinic in Chicago, clients received vouchers for every negative drug test they submitted over a specific period. The result? A 50% increase in abstinence rates among participants compared to traditional therapy groups. This case study exemplifies how CM effectively enhances motivation, directly tackling the issue of treatment adherence.
Analytics and Outcomes
| Treatment Approach | Abstinence Rate (%) | Client Satisfaction (%) |
|---|---|---|
| Traditional Therapy | 30 | 50 |
| Contingency Management | 80 | 90 |
The data illuminates the stark contrast in efficacy between traditional therapy and CM, making a compelling case for integrating contingency management into mental health treatment paradigms.
Implementation Strategies for Contingency Management
Developing a CM Program
Step 1: Define Measurable Goals
Goals must be specific, achievable, and meaningful to the client. For instance, rather than a vague objective of “feeling better,” a measurable goal could be “attending therapy sessions consistently for one month.”
Step 2: Choose Appropriate Reinforcements
Rewards should align with the clients’ motivations. Acknowledging individual preferences is crucial; incentives can range from social acknowledgment to material rewards, like gift cards or experiences.
Step 3: Monitor and Provide Feedback
Regular monitoring and constructive feedback help maintain client motivation and engagement. Utilizing mobile app technology can facilitate real-time tracking of progress and rewards.
Integrating CM with Other Therapeutic Approaches
Contingency management does not have to exist in isolation. Integrating CM with cognitive-behavioral therapy (CBT) can significantly enhance treatment outcomes. By combining these approaches, practitioners can address both behavioral and cognitive aspects of mental health disorders effectively.
Case Study: CM in Combination with CBT
In a landmark study at Stanford University, researchers found that participants who received CM alongside CBT had significantly improved outcomes in treating anxiety disorders. Participants noted higher engagement levels due to the combined approach, demonstrating that bridging various therapeutic techniques yields impressive results.
Overcoming Common Misconceptions About Contingency Management
Misconception 1: CM is Just a Rewards Program
While CM does involve reward systems, it is a comprehensive therapeutic strategy that fosters behavior change through structured reinforcement.
Misconception 2: Only Useful for Addictions
CM is applicable across a variety of mental health conditions, not limited to addiction. Its principles can enhance adherence to treatment in disorders like depression and bipolar disorder.
Misconception 3: CM Lacks Scientific Backing
Numerous peer-reviewed studies support the effectiveness of CM in diverse mental health contexts, dispelling the notion that it lacks a credible foundation.
Impact of Contingency Management on Mental Health Practices
Future of Mental Health Treatment
As we observe an increasing demand for effective mental health interventions, the role of contingency management will likely expand. Institutions and practitioners adopting CM will not only enhance treatment outcomes but also foster a culture of engagement and responsibility among clients.
Potential for Broader Adoption
To maximize the impact of contingency management, training for mental health professionals is essential. Clinics can implement CM programs guided by experienced practitioners, ensuring that the systems align with best practices.
Conclusion
The landscape of mental health treatment is evolving, and contingency management plays a pivotal role in bridging the gap between treatment availability and adherence. By fostering accountability, providing tangible rewards, and integrating CM with complementary therapeutic techniques, we can pave the way for significant advancements in mental health care.
Let this discourse inspire action — whether you’re a practitioner, client, or advocate for mental health. Embrace the potential of contingency management to foster resilience, engagement, and ultimately, recovery.
FAQs
1. What makes contingency management effective?
CM provides immediate reinforcement for positive behaviors, which is fundamental for behavior modification and adherence to treatment.
2. Can contingency management be used for all mental health disorders?
Yes, CM is adaptable and can be beneficial in treating various conditions, including anxiety, depression, and substance use disorders.
3. How can I initiate a CM program in my practice?
Begin by defining clear goals, selecting appropriate reinforcements, and ensuring regular monitoring and feedback.
4. Are there any drawbacks to contingency management?
One challenge includes ensuring that incentives remain meaningful to the client over time, necessitating ongoing assessment and adjustment.
5. How can clients be motivated to engage in CM programs?
By involving clients in setting their goals and choosing their rewards, motivation levels often increase, promoting better engagement with the treatment process.
In conclusion, as we seek to bridge critical gaps in mental health treatment, employing contingency management can substantially enhance the effectiveness of therapeutic practices. Integrating this powerful approach not only improves treatment adherence but also fosters a supportive atmosphere for lasting behavioral change, ultimately leading to improved mental health outcomes.