Introduction: Understanding Sensitization
Have you ever sneezed in a field of blooming flowers or experienced a sudden rash after eating certain foods? These reactions may seem fleeting, but they might be clues to a bigger picture regarding your health. The complex relationship between allergies and autoimmune responses is rooted in a foundational process known as sensitization. In this article, we’ll explore the intricate journey from simple allergic reactions to the more severe and chronic manifestations of autoimmune diseases, revealing how sensitization plays a pivotal role in each phase.
In a world where chronic illnesses are on the rise, understanding this relationship can empower individuals to take control of their health. Let’s dive into the fascinating mechanics of sensitization and its profound effects on our immune system.
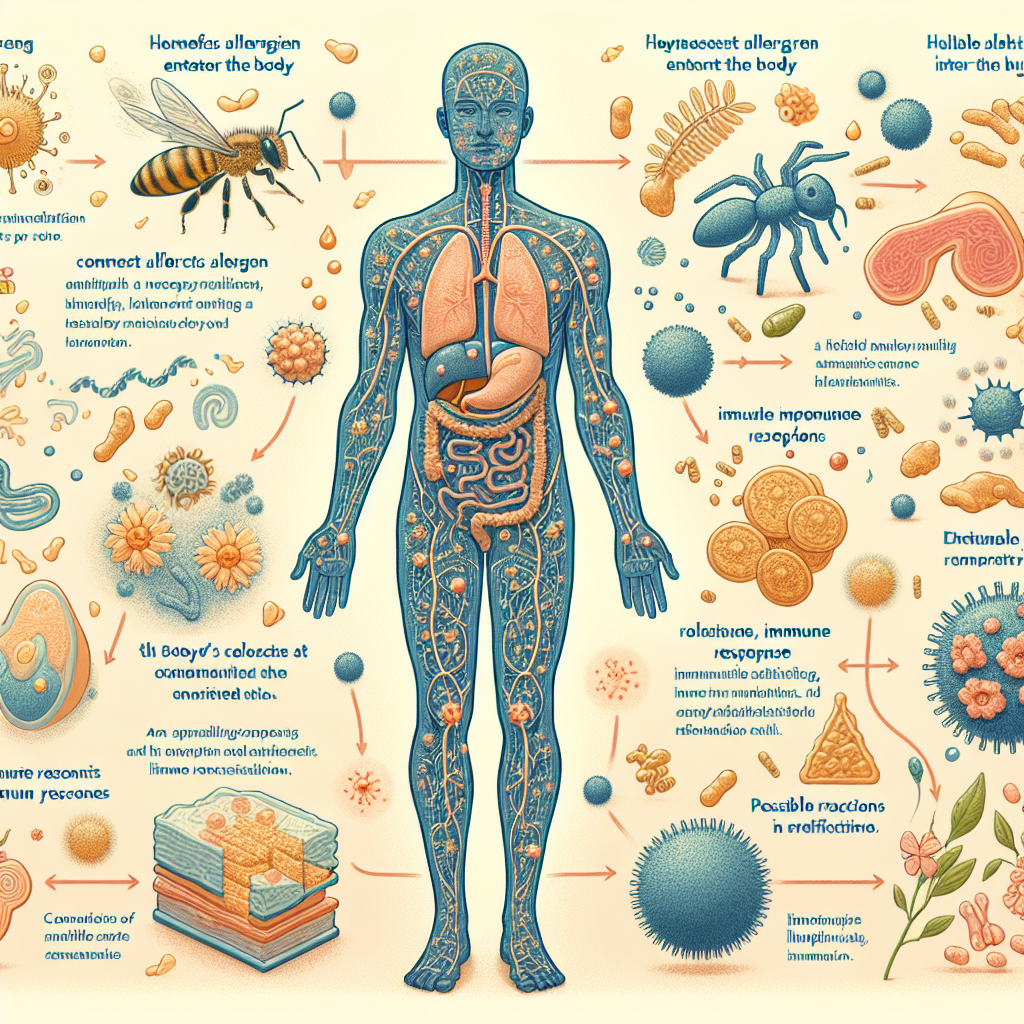
What is Sensitization?
Sensitization is an immune system response where the body becomes "aware" of a particular allergen or trigger after initial exposure. This awareness leads to the production of specific antibodies. The next time the allergen is encountered, a more aggressive immune response occurs, leading to various symptoms — ranging from mild to severe.
Types of Sensitization
Understanding the different types of sensitization can help elucidate how various health issues are related to allergies and autoimmune disorders.
IgE-Mediated Sensitization: This is what most people think of when they consider allergies. It involves Immunoglobulin E (IgE) antibodies binding to allergens, leading to immediate hypersensitivity reactions such as hives or anaphylaxis.
- T-cell Mediated Sensitization: In this slower response, T cells recognize allergens and mount an immune response. This type of sensitization can be involved in autoimmune diseases, where the immune system mistakenly attacks the body’s own tissues.
Both types play crucial roles in the spectrum of health issues ranging from allergies to autoimmune diseases.
The Connection Between Allergies and Autoimmunity
The Immune System: A Two-Edged Sword
The immune system is not just a guardian against infections; it also aims to differentiate between harmful substances and those that are benign. While allergies represent an overreaction to harmless substances, autoimmune diseases signify a misdirected immune response.
Case Study: Peanut Allergies vs. Lupus
In children, peanut allergies may be a result of over-reactive IgE-mediated sensitization, leading to acute reactions. In contrast, systemic lupus erythematosus (SLE) is an autoimmune condition where an individual’s T cells mistakenly target healthy cells, resulting in systemic inflammation and complications.
Analysis
These two conditions highlight the spectrum of immune responses. While one is an exaggerated reaction to a seemingly benign substance, the other is a dangerous attack on the body’s own cells. Understanding this can provide insight into treatment methods and preventative strategies.
The Role of Environmental Factors
Environmental factors such as pollution, diet, and microbial exposure influence the likelihood of sensitization. For instance, urbanization and lifestyle changes may contribute to the rising incidence of allergic diseases and autoimmune conditions.
| Factor | Impact on Sensitization |
|---|---|
| Pollution | Increases IgE sensitization |
| Diet | Affects gut microbiota and immune modulation |
| Microbial Exposure | Helps develop a tolerant immune response |
The Progression from Allergic Reactions to Autoimmune Disorders
Initial Sensitization: A Perfect Storm
The journey from allergies to autoimmune responses often begins with initial sensitization. The body is exposed to allergens, triggering an immune response that can be classified as a simple allergy.
Key Triggers
- Pollen: Seasonal allergic rhinitis can serve as a precursor for autoimmune sensitivities.
- Food Allergens: Proteins found in foods like gluten can later trigger autoimmune responses in susceptible individuals.
The Tipping Point: From Allergies to Autoimmunity
In certain individuals, repeated exposure to allergens can lead to an abnormal immune response, creating a scenario where the body begins to attack itself. This shift can transform mild allergies into serious autoimmune diseases.
Case Study: Celiac Disease
Celiac disease exemplifies this progression. Individuals initially diagnosed with gluten sensitivity may develop an autoimmune reaction affecting the intestines, leading to serious long-term health consequences if not managed properly.
Analysis
The shift from a benign allergic response to a chronic autoimmune condition underscores the need for proactive monitoring and lifestyle adjustments in at-risk individuals.
Recognizing the Symptoms: When to Seek Help
Allergic Responses
Common symptoms of allergies include:
- Sneezing
- Itchy or watery eyes
- Rashes or hives
Autoimmune Symptoms
Conversely, autoimmune disorders often present with:
- Fatigue
- Joint pain
- Swelling or inflammation
- Fever
It’s essential to seek medical advice if you notice a progression in symptoms or their severity, as early intervention can be critical.
Stress: The Hidden Trigger
The Immune Connection
Chronic stress has been implicated in worsening both allergies and autoimmune conditions. Stress can lead to hormonal changes that may exacerbate immune responses.
Case Study: Asthma
Individuals with asthma may find their symptoms flare up during stressful periods due to increased inflammation and airway constriction. Stress management techniques can provide considerable relief.
Analysis
Addressing stress not only enhances mental well-being but can also mitigate physical health issues stemming from either allergies or autoimmune responses.
Managing Sensitization: Practical Strategies
Dietary Interventions
- Elimination Diets: Identifying and removing potential allergens can significantly reduce sensitization and associated symptoms.
- Anti-inflammatory Foods: Incorporating foods rich in omega-3 fatty acids, antioxidants, and probiotics can support immune function.
Environmental Management
Reducing exposure to known allergens can decrease sensitization responses. For example, using air purifiers and implementing strict cleaning regimens can create a safer living environment.
Lifestyle Adjustments
Incorporating stress management techniques such as mindfulness, yoga, or regular exercise can markedly improve the quality of life for those affected by allergies and autoimmune diseases.
Conclusion: Empowering Health Through Knowledge
From Allergies to Autoimmune Responses: The Role of Sensitization in Health reveals a vital connection that can empower individuals. By understanding the dynamics of sensitization, one can take proactive measures to manage and potentially mitigate adverse health effects.
In a world filled with varying allergens and stressors, a blend of smart dietary choices, environmental controls, and lifestyle modifications can pave the way towards a healthier existence.
Are you ready to take charge of your health? Awareness is key, and each small step can lead to profound changes in your overall well-being.
FAQs
What exactly is sensitization?
- Sensitization is the process by which the immune system identifies and reacts to an allergen, leading to hypersensitivity upon subsequent exposures.
Are allergies and autoimmune diseases the same?
- No, allergies result from an overactive immune response to harmless substances, while autoimmune diseases involve the immune system mistakenly attacking the body’s own tissues.
How can I tell if my symptoms are allergies or autoimmune?
- Allergies often present with clear triggers (like pollen or certain foods) and immediate symptoms, while autoimmune disorders tend to be more chronic and may vary significantly in symptoms over time.
What role does genetics play in these conditions?
- Genetics can contribute to both allergy and autoimmune predisposition. If these conditions run in your family, you may be at an increased risk.
- Can lifestyle changes really impact these conditions?
- Yes, adopting a healthier lifestyle through proper diet, stress management, and reducing exposure to allergens can significantly improve symptoms and overall health.
By gaining knowledge about how sensitization operates, individuals can embark on a journey towards better health, informed by science and personal experience.