Introduction
Chronic illness management is a journey—one that is often fraught with challenges and complexities but can lead to remarkable personal growth. In our fast-paced world, where solutions are often sought in quick-fix pharmaceuticals, finding balance through integrative approaches to chronic illness management has emerged as a beacon of hope. This article explores holistic and evidence-based strategies, emphasizing the significance of personalized care pathways that honor both the body and mind.
Understanding Chronic Illness
What is Chronic Illness?
Chronic illness refers to long-term health conditions, such as diabetes, arthritis, and cardiovascular diseases, which typically extend for three months or more. Unlike acute illnesses, which often resolve quickly, chronic conditions require ongoing management and adaptation.
The Importance of a Holistic Perspective
When managing chronic illnesses, traditional medical approaches often focus solely on symptom relief. However, integrative approaches to chronic illness management emphasize the interconnectedness of physical, emotional, and social well-being. They advocate a more comprehensive system of care that goes beyond medications.
Finding Balance: Integrative Approaches to Chronic Illness Management
1. Mind-Body Practices
Mind-body practices, such as yoga, meditation, and tai chi, have gained recognition for their ability to reduce stress and improve physical health. According to a recent study, patients who engaged in mind-body interventions reported a significant reduction in pain levels.
Case Study:
Sarah is a 32-year-old with fibromyalgia. After integrating yoga and mindfulness meditation into her routine, she experienced a dramatic reduction in pain and fatigue. By focusing on her mental state, she found more power over her physical symptoms.
Analysis
Sarah’s story illustrates the profound impact of mind-body practices. Engaging in activities that foster mindfulness can allow patients to develop resilience and cope better with their conditions.
2. Nutrition and Diet
The saying "you are what you eat" holds substantial weight, particularly for patients grappling with chronic illnesses. Personalized nutrition plans that cater to individual needs can significantly improve health outcomes.
The Role of Anti-Inflammatory Foods
Foods rich in omega-3 fatty acids, antioxidants, and dietary fiber can combat inflammation—an underlying culprit in many chronic diseases.
Table 1: Anti-Inflammatory Foods
| Food Type | Examples | Benefits |
|---|---|---|
| Omega-3 Sources | Salmon, walnuts, flaxseeds | Reduces inflammation |
| Antioxidant-Rich | Berries, leafy greens, nuts | Protects against cellular damage |
| High-Fiber Foods | Whole grains, legumes | Supports digestive health |
Case Study:
John, diagnosed with type 2 diabetes, overhauled his diet by incorporating more whole foods and reducing processed sugars. Within three months, his blood sugar levels stabilized, showcasing the power of nutrition in managing chronic illness.
Analysis
John’s transformation emphasizes the essential role of nutrition in chronic illness management. Tailoring dietary choices can empower patients to take charge of their health.
3. Physical Activity
Regular physical activity mitigates symptoms and contributes to overall health. Exercise programs should be customized to fit different abilities and medical recommendations.
Benefits of Exercise:
- Improved cardiovascular health
- Enhanced mood and emotional well-being
- Increased mobility and strength
Case Study:
Emily, who has rheumatoid arthritis, found relief through an individualized exercise regimen comprising low-impact aerobics and strength training. Over time, she experienced less joint stiffness and improved energy levels.
Analysis
Emily’s journey underscores that with the right guidance, individuals with chronic illnesses can engage in physical activity to enhance their well-being.
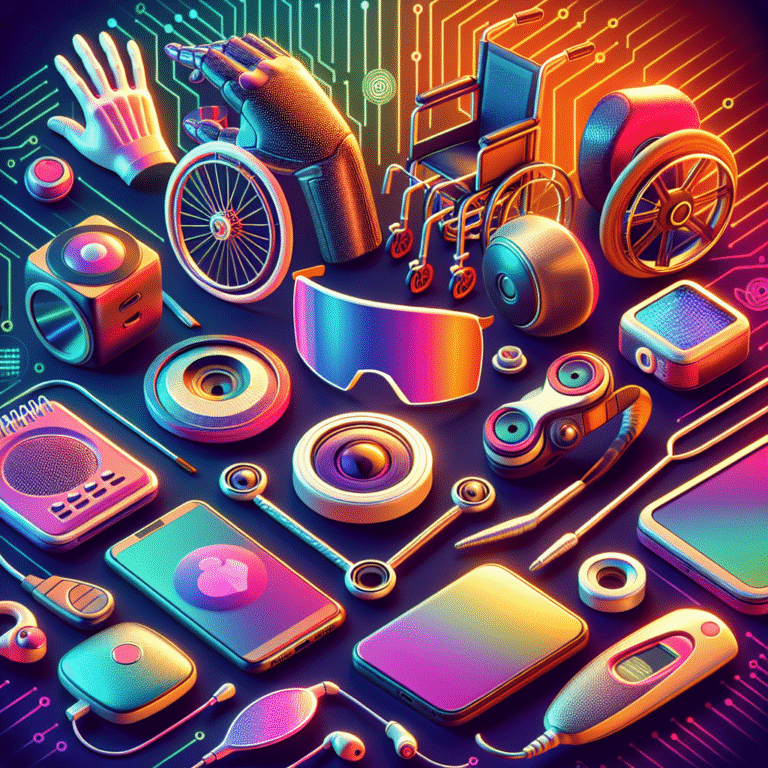
4. Complementary Therapies
Complementary therapies, including acupuncture, chiropractic care, and aromatherapy, can provide additional support in managing chronic illnesses.
Case Study:
Tom, suffering from migraine headaches, found relief through regular acupuncture sessions. Not only did the therapy reduce the frequency of his migraines, but it also helped him manage stress better.
Analysis
Tom’s experience highlights the effectiveness of complementary therapies in providing holistic care. These therapies can enhance traditional medical interventions.
5. Emotional Support and Community
The emotional toll of chronic illness can be overwhelming. Building a support network and connecting with others facing similar challenges can foster resilience.
Group Therapy and Support Networks
Participating in group therapy or support networks can help patients process their emotions, share experiences, and find encouragement.
Case Study:
Lisa, diagnosed with lupus, joined a local support group. Through shared stories, she gained invaluable strategies and emotional support that helped her cope with her diagnosis.
Analysis
Lisa’s story is a testament to the strength found in community. Emotional support is a crucial component of integrative chronic illness management.
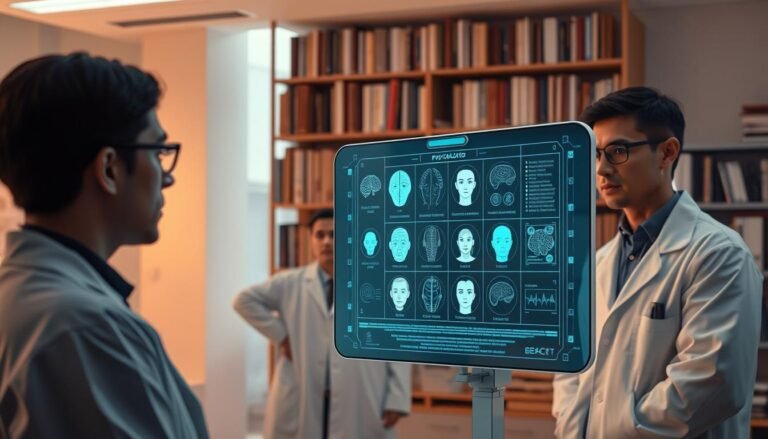
6. Integrative Medicine Teams
A multidisciplinary approach to chronic illness management fosters effective collaboration between various healthcare providers, such as doctors, nutritionists, and mental health professionals.
Benefits:
- Comprehensive treatment plans
- Coordinated care strategies
- Increased patient satisfaction
Case Study:
Mark’s journey with chronic pain transformed when he began working with a team of specialists. His integrative medicine team developed a holistic approach that considered all facets of his health, resulting in a marked improvement in his quality of life.
Analysis
Mark’s experience illustrates the advantages of an integrative care model. When healthcare practitioners work together, patients often report improved health outcomes.
Conclusion
Finding balance through integrative approaches to chronic illness management is not just beneficial—it’s essential. From mind-body practices and nutrition to community support and comprehensive care teams, these strategies empower individuals to navigate their health journeys more effectively. Chronic illness may present challenges, but with a well-rounded approach, patients can reclaim control over their lives.
FAQs
1. What are integrative approaches to chronic illness management?
Integrative approaches encompass a holistic view of health, combining conventional medicine with complementary therapies, nutrition, and lifestyle changes to optimize well-being.
2. How can nutrition impact chronic illness?
A well-balanced diet can reduce inflammation, manage symptoms, and improve overall health, making it a vital component of chronic illness management.
3. Are mind-body practices effective for everyone?
While many individuals find relief through mind-body practices, effectiveness can vary. Personalization and individual preferences play key roles.
4. What role does emotional support play in managing chronic illness?
Emotional support can significantly enhance coping mechanisms, relieve stress, and improve overall quality of life, making it critical for individuals with chronic conditions.
5. How can I get started with an integrative approach?
Consult with healthcare providers to develop a personalized plan incorporating various elements like nutrition, exercise, mind-body practices, and emotional support tailored to your specific needs.
By embracing a multifaceted approach, patients can find balance in managing chronic illnesses, leading to more fulfilling lives despite the challenges they face.