Introduction
Imagine you are a healthcare professional encountering a patient whose symptoms seem exaggerated or unsubstantiated. How do you navigate the thin line between providing compassionate care and ensuring the integrity of your practice? The Ethical Dilemmas of Malingering Detection: Balancing Care and Credibility is a vital issue in modern medicine, impacting not only the diagnosis but also the quality of care received by patients. As the healthcare landscape evolves, the challenges of discerning genuine medical conditions from feigned ones become increasingly complex. This article delves into these ethical dilemmas, offering insights, real-world case studies, and a roadmap for healthcare professionals grappling with these critical challenges.
Understanding Malingering: A Brief Overview
Malingering is defined as the intentional production of false or exaggerated symptoms, motivated by external incentives such as financial gain, avoidance of responsibilities, or receiving drugs. While it exists on a spectrum, distinguishing genuine cases from those of malingering presents significant ethical challenges. The implications of misdiagnosing a malingerer can have far-reaching effects, undermining trust and healthcare efficacy.
Case Study: The Veteran’s Dilemma
Consider a case involving a war veteran seeking disability benefits. He presents with severe PTSD symptoms that, while troubling, raise suspicion among healthcare providers. The ethical dilemma here involves weighing his genuine psychological distress against potential motivations for exaggeration. Does the chance of malingering complicate the responsibility of accurately diagnosing and treating his condition?
The Ethical Implications of Malingering Detection
Detecting malingering is not simply a matter of identifying deceptive patients; it also raises profound ethical questions.
The Impact of Misdiagnosis
Misdiagnosis can lead to unnecessary treatments, emotional distress, and even financial repercussions for patients. False accusations of malingering may erode patient-provider relationships, leading to a breakdown in trust, which is essential for effective treatment.
Table 1: Potential Consequences of Misdiagnosing Malingering
| Consequence | Impact on Patient | Impact on Provider |
|---|---|---|
| Emotional distress | Increased anxiety | Legal liability |
| Financial repercussions | Loss of benefits | Ethical scrutiny |
| Delay in appropriate treatment | Worsening of condition | Decreased credibility |
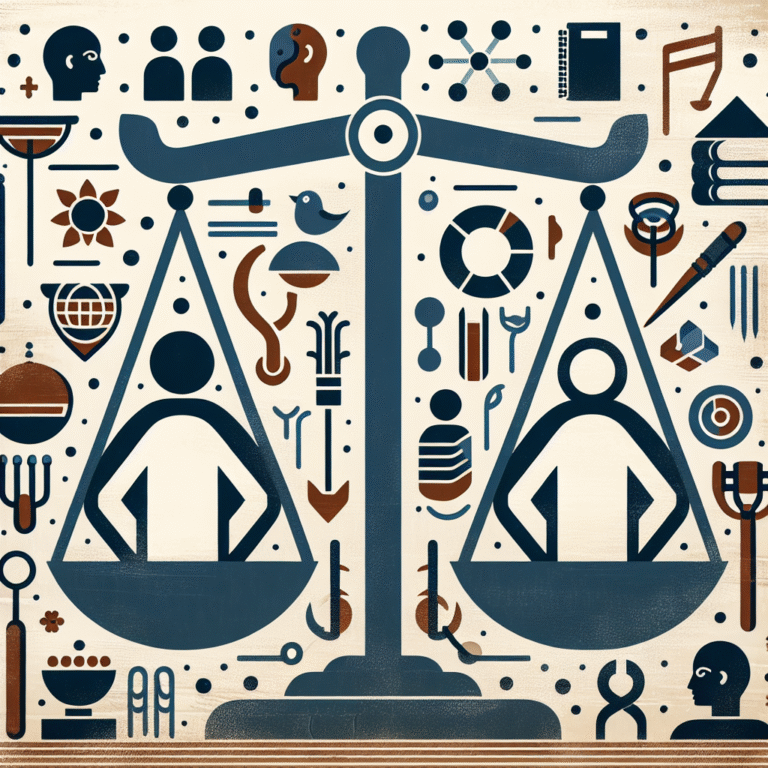
Balancing Care and Credibility
Healthcare providers are tasked with a dual responsibility: to provide care while maintaining the integrity of their profession. This balance can often feel like a tightrope walk where one misstep can lead to serious ethical consequences.
Techniques for Malingering Detection
Understanding the methods employed to detect malingering can help professionals maintain ethical standards while ensuring proper care.
Psychological Assessments
Psychological assessments can reveal inconsistencies in reporting symptoms, helping to determine the truth behind a patient’s claims. However, interpreting these assessments requires sensitivity to the underlying issues faced by the patient.
Clinical Interviews
A thorough clinical interview can expose discrepancies in accounts of symptoms and duration. It’s essential to approach these interviews empathetically to avoid alienating the patient.
Functional Assessments
Functional assessments assess a patient’s ability to perform everyday tasks and can provide insight into whether claims of dysfunction are legitimate.
Cases When Ethics Clash
Case Study: The Chronic Pain Patient
Consider a patient with a history of chronic pain who seeks opioid prescriptions regularly. Healthcare providers may suspect malingering due to the patient’s frequent requests, which puts them in an ethical dilemma. Should they risk enabling addiction by continuing prescriptions, or should they confront the patient with skepticism, potentially worsening their psychological state?
Ethical Considerations
This scenario underscores the importance of a multi-faceted approach in detection. Providers should consider not only the potential for malingering but also the impact of their decisions on the patient’s overall well-being.
Real-World Applications: Best Practices for Providers
Building Rapport
Establishing trust is vital for successful treatment. Open communication fosters an atmosphere where patients feel comfortable expressing their concerns, mitigating fears of being labeled as malingerers.
Multi-Disciplinary Approaches
Utilizing a team of professionals—psychologists, physical therapists, and social workers—can provide a comprehensive view of a patient’s condition, aiding in ethical decision-making.
Ongoing Education
Education on the ethical dilemmas surrounding malingering detection should be regular and comprehensive. Continuous learning helps providers stay informed about the latest techniques and ethical standards in their field.
Conclusion
The Ethical Dilemmas of Malingering Detection: Balancing Care and Credibility presents a complex landscape that healthcare professionals must navigate diligently. As emphasized throughout this article, the intertwining of ethical standards with patient care requires a delicate balance. Malingering detection does not merely focus on identifying fraudulent behaviors; it is about understanding the human experience behind those behaviors.
Healthcare providers should leverage effective communication, education, and multi-disciplinary approaches to create an environment that safeguards both the integrity of practice and the welfare of patients. Ultimately, the principles of empathy and ethical responsibility should guide practitioners as they handle these challenging dilemmas.
FAQs
1. What is malingering?
Malingering involves the deliberate fabrication of symptoms for personal gain, such as financial compensation or avoidance of work.
2. How can healthcare providers detect malingering?
Common methods include psychological assessments, clinical interviews, and functional assessments to evaluate the authenticity of reported symptoms.
3. What are the ethical considerations in malingering detection?
Providers must balance the risk of misdiagnosing genuine patients against the need to prevent fraud, which requires sensitivity and careful assessment.
4. Can malingering affect healthcare costs?
Yes, malingering can increase healthcare costs due to unnecessary treatments and diagnostics, which could be avoided with accurate detection.
5. How can trust be built between healthcare providers and patients suspected of malingering?
Open, honest communication and empathy are key strategies for building rapport, encouraging patients to feel comfortable discussing their concerns without fear of judgment.
By contextualizing The Ethical Dilemmas of Malingering Detection: Balancing Care and Credibility within real-world applications and frameworks of best practices, this article provides a unique resource for healthcare professionals navigating this essential aspect of patient care.